This is the most common type of headache a person suffers from.
The pain is typically experienced as mild to moderate and the pain is often described as a feeling of tightening around the whole head. This headache is caused mainly by muscular origin where some of the muscles are in spasm and have active trigger points causing your headache. Stress can aggravate or trigger a tension headache.

Physiotherapy may include myofacial release massage and dry needling therapy to release muscle spasms and trigger points. The cervical and thoracic spine will be assessed for any stiffness. Stretches and mobilisation exercises may be specifically prescribed as well as some posture correction and strengthening as determined by the individuals examination. Taping may be used to deactivate over active muscles.

This headache is often experienced to be moderate to severe in intensity, and may be chronic in nature. The headache often responds poorly to analgaesic medicine. The area of pain is often on one side of the head. It can change between left and right side and can be on both sides. The headache is caused by muscle spasm as well as joint pathology- usually there is pain and stiffness on palpation of one or more of the cervical joints from level C1- C3. There is a sensory stimulus of the trigeminal nerve, which allows for the area of pain experienced.
Physiotherapy treatment will involve mobilisation of the affected cervical joints as well as myofacial release and, or deep dry needling of the muscle spasms and trigger points. Down regulation of the nervous system may be indicated and be part of the rehabilitation. Other techniques such as taping, electrotherapy and heat may be used. Exercises will be prescribed to stretch tight muscles, mobilise stiff joints and strengthen weak muscles.
Temporomandibular Joint (TMJ/ Jaw) dysfunction- Your TMJ is the most used joint in the body. Your TMJs (jaw joints) are involved with eating, talking, breathing and, probably most importantly, expressing our feelings and emotions. When things go wrong with your TMJ it is known as Temporomandibular Disorder (TMD). TMD sufferers are often teeth grinders or clenchers.
You may or may not even experience jaw pain or tenderness with TMJ dysfunction. The most common symptoms include:
⦁ jaw clicking
⦁ jaw popping
⦁ grinding
⦁ limited jaw opening, or jaw deviation while opening (which you can observe in a mirror)
⦁ an inability to fully clench your jaw.
⦁ Headaches and upper neck pain
⦁ Ear pain or ringing
Many things can contribute to TMD
Contributory factors include:
⦁ Mandibular malalignment secondary to occlusal appliance or orthodontic treatment.
⦁ Removal of wisdom teeth,
⦁ Prolonged mouth opening such as during a dental procedure,
⦁ Poor head on neck (cervical) posture,
⦁ Myofascial trigger point pain,
⦁ Stress, and
⦁ Whiplash and other less common causes include: trauma (e.g., blow to the chin), infection, polyarthritic conditions, tumors, and anatomical abnormalities.
TMJ Opening problems include:
⦁ Muscle disorder,
⦁ TMJ (joint) disorder: hypermobility, stiffness or arthritis,
⦁ TMJ disc displacement disorder: intermittent or permanent lock, or a
⦁ Poor head on neck posture
TMJ Closing problems include:
⦁ a locked open joint, which can be manipulated open, or an
⦁ occlusion problem, which may require a bite assessment from your dentist.
TMJ Treatment?
After your TMJ assessment your physiotherapist will commence treatment targeting specific problems found on assessment. Physiotherapy treatment can include myofacial trigger point release of jaw muscles such as masseter and contributing neck muscle spasms. Deep dry needling may be used as well as mobilisation techniques of the TMJ.
Head on neck posture has been found to have a greater affect on Your TMJ dysfunction than on neck pathology- as such,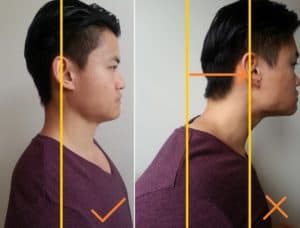 posture correction is usually a big part of the rehabilitation process. Physiotherapy is normally successful for the treatment of TMJ opening disorders due to the problem being a movement disorder that is affected by your muscle and joint control.
posture correction is usually a big part of the rehabilitation process. Physiotherapy is normally successful for the treatment of TMJ opening disorders due to the problem being a movement disorder that is affected by your muscle and joint control.
Your dentist is usually involved in the management of TMJ closing disorders such as bruxism due to the the addition of teeth occlusion. In some cases, an occlusion splint or bite plate may be recommended.
NECK PAIN- Neck pain is a common musculoskeletal disorder which can present itself in a number of ways. More often than not, neck pain is localised to the neck region itself, but it can be more widespread and travel into the shoulders and arms- this may sometimes make you worry that you have a pinched nerve.
There might even be associated headache and/or a restriction in range of movement. It is rare that neck pain has a more serious cause.
Neck pain is becoming more common due to the high stress lives we le ad, our increasingly sedentary lifestyles, and due to the sustained poor postures we adopt on our tablets, phones and computers.
ad, our increasingly sedentary lifestyles, and due to the sustained poor postures we adopt on our tablets, phones and computers.
Typically physiotherapy involves releasing any tight and painful muscles by method of myofacial release, deep dry needling, electrotherapy, exercise, heat and taping. Your cervical and thoracic spine will be assessed for pain and stiffness and these joints will be mobilised. At this practice we often use Mulligan and Maitland mobilistation techniques to gain range of motion at a joint segment. Exercises will be prescribed to strengthen and stretch muscles found to be contributing to the neck pain.
This occurs with pathologies that causes symptoms on the nerve roots. Those can be compression, irritation, traction, and a lesion on the nerve root caused by either a herniated disc, foraminal narrowing or degenerative spondylitic change (Osteoarthritic changes) leading to stenosis of the intervertebral foramen.
Most of the time cervical radiculopathy symptoms appear unilaterally, however it is possible for bilateral symptoms to be present if severe bony spurs are present at one level, impinging/irritating the nerve root on both sides. Pain is often constant, severe and lancinating in nature. If peripheral radiation of pain (pain into the arm), weakness or pins and needles are present, the location of the pain will follow back to the specific affected nerve root.
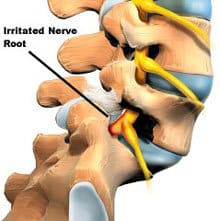
Cervical radiculopathy is dysfunction of a nerve root in the cervical spine. It is a broad disorder with several mechanisms of pathology and it can affect people of any age, with peak prominence between the ages of 40 and 50. We were made with strong spines, designed to move, hence this condition is relatively uncommon, with a reported prevalence of 83 people per 100,000. Not all neck pain referring to the arm indicates that a nerve is impinged- some trigger points can refer into these areas and one needs to also look at whether you may have shoulder pathology.
Where a nerve root is compressed it can cause a combination of factors: inflammatory mediators, changes in vascular response and intraneural oedema (swelling) which causes radicular (referred) pain. A nerve root can be compressed without causing pain- but one may experience sensory and motor dysfunction such as changes in sensation and weakness or changes in reflexes when tested.
Physiotherapy is often successful in treating neck pain with radiculopathy when the main cause is an inflammatory irritation of the nerve root or with mild disc pathology such as a disc bulge irritating a nerve root. Often physiotherapy is combined with a strong cocktail of medication targeting the pain and inflammation prescribed by your doctor. In this case we target releasing muscular nerve entrappers in the area, such as the scalene muscle to decrease tension on the nerve root. We also release any muscle spasms and trigger points in the neck and shoulder area that can be adding to the pain experience. We add gentle neural sliders to mobilise the nerve root and improve blood supply for healing. We also specifically mobilise affected levels of the cervical spine to improve mobility at that level and decrease any ongoing inflammatory drive caused from a joint not moving properly. Gentle exercises to improve posture may be important if poor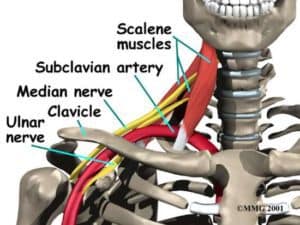 head on neck posture seems to be a contributor. The goal is to offload the nerve root by changing some of the bio-mechanics so that the inflammation can subside in combination with the medication and maintaining movement. You will feel worse if you don’t move your neck or are in a soft neck collar. All the latest research indicates that some movement is very important in decreasing pain. Your physiotherapist will help you with how much movement is too much and what movements may give the most benefit.
head on neck posture seems to be a contributor. The goal is to offload the nerve root by changing some of the bio-mechanics so that the inflammation can subside in combination with the medication and maintaining movement. You will feel worse if you don’t move your neck or are in a soft neck collar. All the latest research indicates that some movement is very important in decreasing pain. Your physiotherapist will help you with how much movement is too much and what movements may give the most benefit.
An MRI is the imaging of choice if a nerve root compression is suspected. The physiotherapist will refer you to an orthopaedic or neurosurgeon specialist for management if this is suspected after evaluation.
Sometimes surgery is the only option, but sometimes if pathology is mild the physiotherapist and the specialist combine conservative management to see if surgery can be avoided. In this case conservative management is usually given a maximum of 6 weeks to relieve symptoms.
If conservative management is successful in getting rid of the symptoms then one must focus on strengthening your neck to offload the spine and to get segmental stability at that level while maintaining flexibility. This is the only way to slow down degeneration at the affected level. If surgery is the only option the post operative physiotherapy is again important to strengthen the spine. This is to prevent instability at the level above and below the fused segment which may at a later stage then cause need for another fusion if left to degenerate.
Lower back pain is very common. Eighty percent (80%) of people will experience lower back pain at some stage in their life. It is one of the most common reasons for people missing work and seeing a doctor or physiotherapist. Fortunately, most back pain is caused by musculoskeletal conditions and can be treated with great success.
Acute lower back pain is most often caused by a sudden injury to the muscles and ligaments supporting the back. The pain may be caused by muscle spasms or a strain or tear in the muscles and ligaments. Occasionally the cause may be more serious, but this is more rare.
Causes of Sudden Lower Back Pain:
- Muscle Strain or Muscle Spasm
- Lumbar Disc Injury
- Compression fractures eg. Osteoporosis
- Nerve irritation or impingement (sciatica)
- Cancer of the spine
What Causes Lower Back Pain?
Lower Back Pain is categorised into the following categories:
1. Specific Spinal Pathologies (<1% of cases)
Some conditions that cause back pain do require urgent and specific referral and treatment. These can include spinal infections, cancer/malignancy, spinal arthropathies (eg rheumatoid arthritis or ankylosing spondylitis), cauda equina syndrome or spinal fractures. These conditions do require early diagnosis and prompt referral to the appropriate medical specialist. Luckily these conditions account for less than 1% of back pain sufferers, but you don’t want them missed.
2. Radicular Syndromes (5-10% of cases)
Lower back pain can result from structural damage that can irritate or pinch a nerve. Researchers believe that radicular syndrome causes 5-10% of the presentations of back pain to general practitioners. The most common nerve that can be pinched in the lower back is your sciatic nerve. You may be diagnosed with sciatica if you are suffering radicular pain down the back of your leg due to a back injury. While the sciatic nerve is the most common nerve that can be affected by a spinal injury any nerve can be affected such as your femoral nerve (pain will be felt in the front or side of your thigh).
Many injuries can cause radicular pain, such as a herniated disc , facet joint sprain, spondylolisthesis, spondylolysis, degenerative disc disease, spondylosis (arthritis), and back ligament sprain. These can all contribute to or cause radicular pain syndrome due to swelling or space occupying material next to the spinal nerve. The nerve is either irritated (radicular pain) or pinched/compressed (radiculopathy).
An irritated nerve often responds well to physiotherapy, especially when the cause is a facet joint sprain, degenerative disc disease, disc bulge, arthritis, ligament sprain or muscular nerve entrapment ie. in piriformis or Iliopsoas muscle spasm. Most of the time physiotherapy is combined with specific medication prescribed by your doctor to treat the nerve pain and inflammation.
Lumbar radiculopathy can result in muscle weakness that can inhibit walking and the pain is often very disabling. Spinal stenosis is a slightly different condition and relates to compression of the spinal canal. Spinal stenosis is usually more prevalent as you age. You may find relief when bending forward and symptoms may be felt in both legs. Often surgical intervention is required in these cases.
3. Non-Specific Lower Back Pain (90-95% of cases)

Non- specific lower back pain is the diagnostic term used to classify sufferers of lower back pain where no specific structure has been injured. It is really a diagnosis of exclusion. In other words, your medical practitioner has excluded specific spinal pathologies and any of the radicular syndromes mentioned above as the cause of your back pain or symptoms.
Fortunately, these conditions account for approximately 90-95% of the lower back pain causes and they can nearly always be successfully managed conservatively and without the need for surgery. Most improve within two to six weeks. Physiotherapy techniques such as manual therapy and back exercises can help relieve symptoms quicker.
Most lower back pain causes are musculoskeletal in origin and known as non-specific low back pain (NSLPB). The causes of lower back pain are numerous but roughly fall into either a sudden (traumatic) or sustained overstress injuries.
Most people can relate to traumatic injury such as bending awkwardly to lift a heavy load that then causes painful muscle spasm or strain. However, sustained overstress injuries (eg poor posture) are probably more common but also easier to prevent. In these cases, normally positional stress or postural fatigue creates an accumulated affect which overloads your lower back support structures over an extended period of time. This often results in muscle spasm, muscle sprain or ligament strain, which can result in some stiffness of the lumbar spine as well as referred pain in the leg due to infammation near a nerve root or as part of a trigger points referral pattern. Physiotherapy releases any tight muscles and trigger points with myofacial release, deep dry needling, and exercise. Spinal mobilisation and mobilisation exercises are performed to improve mobility where there may be spinal stiffness. Strengthening exercises are taught to maintain good spinal health and mobility. Taping may be used initially to assist with pain relief. Advice and pain neuroscience education may be shared to prevent recurrent episodes of lower back pain.
Piriformis syndrome
Piriformis syndrome is one of the potential causes of lower back pain and pain going down the leg (sciatica). It is one of the areas that needs to be evaluated whenever a person has lower back pain or sciatica. Patients with piriformis syndrome have many symptoms that typically consist of persistent and radiating low back pain, (chronic) buttock pain, numbness, paraesthesia, difficulty with walking and other functional activities such as pain with sitting (especially on hard surfaces), squatting and long standing. Walking can often give some relief to the pain.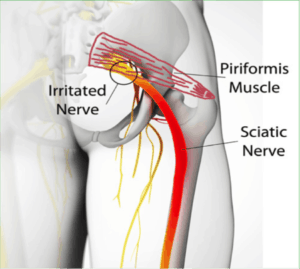
The piriformis muscle can be shortened or in spasm and thereby cause a compression or irritation of the sciatic nerve. This shortened piriformis is often due to a compensation for weak gluteus maximus and medius. Another cause may be prolonged sitting on a hard surface that may compress the nerve and cause irritation of the sciatic nerve.
On evaluation there will be positive neural tension compared to the other leg. There will also be moderate to severe pain on palpation of the piriformis muscle, you may even feel the pain radiate down your thigh.
Physiotherapy will involve releasing tight structures with techniques such as myofacial release, deep dry needling, stretches, neural sliders and strengthening of weak muscles.
Often conservative treatment is successful but occasionally surgical release of the nerve may be required when scar tissue or something physical may be compressing the nerve at the piriformis muscle.
Thoracic Pain
Thoracic Pain (upper back pain ) is common. The function of the thoracic spine and rib cage is to protect your organs. It is also a base for which muscles of the upper limbs, neck and head, vertebral column and pelvis can attach. As it’s main role is stability, this is the least mobile part of your spine.
) is common. The function of the thoracic spine and rib cage is to protect your organs. It is also a base for which muscles of the upper limbs, neck and head, vertebral column and pelvis can attach. As it’s main role is stability, this is the least mobile part of your spine.
Due to all the organs it carries- referral from organs needs to be excluded as the cause of pain. The thoracic spine is also generally the most common area of the spine to suffer from cancer. It is therefore always important to exclude.
Injuries of the thoracic area can vary from traumatic e.g. a fall, to atraumatic e.g. postural fatigue. We often find pain due to prolonged poor posture especially in woman that have large breasts. We also find pain in individuals who have over-active rhomboids and a flattened thoracic spine curve. Following a chest infection the continuous coughing can cause pain and spasm in this area.
The thoracic pain may co exist with neck pain, headaches or shoulder pain- we often treat the thoracic area while
treating these other areas of pain.
A stiff thoracic spine may predispose developing a condition known as chostochondritis.

Physiotherapy often involves mobilising the thoracic spine and the chostovertebral joints (where ribs join the spine) which are found to be stiff. Release of all tight muscles using massage, deep dry needling, stretches, heat and exercises can be done. Rehabilitation is often to improve the posture in this area and maintain mobility.
Chostochondritis
Chostochondritis is inflammation of the cartilage in the rib cage The condition usually affects the cartilage where the upper ribs attach to the breastbone, or sternum, an area known as the sternocostal joint or sternocostal junction.

Chest pa in caused by costochondritis can range from mild to severe, and can refer down the arm. Often cardiac causes are excluded.
in caused by costochondritis can range from mild to severe, and can refer down the arm. Often cardiac causes are excluded.
This condition seems more prevalent in woman, especially large breasted woman. Predisposing factors could be an office job with lots of typing, or if you drive a lot. Often people experienced thoracic pain or stiffness before the chostochondritis started.
Physiotherapy treatment is given in conjunction with anti-inflammatories. Physiotherapy treatment may include ultrasound, laser, and taping of the area to decrease inflammation- but the most important aspect is mobilisation of the thoracic spine and exercises to maintain thoracic mobility and to improve posture to offload the sternocostal junction.
Hip Pain
Some causes of hip pain:
1. Osteoarthritis of the hip
Arthritic pain in the hip is often felt in the groin, but it can refer down into the leg and into the knee. On examination the range of motion of external rotation of the affected hip will be decreased. An x-ray of the pelvis and hip will show arthritic changes. Arthritis in joints is a normal part of the ageing process, and more frequent above the age of 60 years. You can have arthritis without having pain. If you are experiencing pain then you need to learn to manage your symptoms. During flare ups medication prescribed by your doctor can help manage your symptoms. It is a good idea to do what you can to offload your joint: this includes losing any extra weight you may be carrying, and strengt hening the stabilising muscles of the hip joint. Exercise is very important to get that joint lubricating and to maintain mobility and strength. If you don’t move the joint often gets more stiff and the pain worsens. Your physiotherapist can help mobilise the hip joint and give advice on exercise and activity modification to manage your lifestyle and pain.
hening the stabilising muscles of the hip joint. Exercise is very important to get that joint lubricating and to maintain mobility and strength. If you don’t move the joint often gets more stiff and the pain worsens. Your physiotherapist can help mobilise the hip joint and give advice on exercise and activity modification to manage your lifestyle and pain.
If a total hip replacement is indicated then the physiotherapist will rehabilitate post operatively. The goals are to get you walking pain free again and back to your previous function with strengthening the hip and knee stabilisers post operatively as these are very important in balance and a successful outcome.
2. Trochanteric Bursitis of the hip
A bursa is supposed to decrease friction between a tendon and bone, but can become inflamed and cause severe pain. This is often due to a mechanical overload at that area and along with pain management one will need to strengthen and stretch certain muscles that are causing this overload to have a long term benefit. The pain will be felt on the outside of the hip (lateral), over the greater trochanter of the hip. If palpated over the greater trochanter the pain is reproduced. Ice, taping and ultrasound can help with pain manage but the rehabilitation of the weak gluteus muscles is the most important as that is typically the cause.
3. Gluteal Tendinopathy
Gluteal tendinopathy is the most common hip tendonitis (hip tendon injury). It is one of the most common causes of pain on the outside of the hip (lateral).
Your gluteal tendons are the tough fibres that connect your gluteal muscle to your hip bone. A tendon injury may seem to happen suddenly, but usually, it is the result of many tiny tears to the tendon that have happened over time. The most common onset of gluteal tendinopathy is due to poor hip and gluteal muscle control that leads to over stressing of the gluteal tendons, causing pain and hip-pelvis instability.
The most common onset of gluteal tendinopathy is due to poor hip and gluteal muscle control that leads to over stressing of the gluteal tendons, causing pain and hip-pelvis instability.
Continued hip instability can cause you to walk or run with poor control, which causes you hip bursa to become under friction load, leading to trochanteric bursitis as well.
While often found in athletes this is also common in menopausal woman who no longer have the oestrogen levels they had before to protect there tendons. A lot of woman will hang on there hips when standing and this causes strain on these gluteal structures. Another cause may be a stretching program where the hip is repetitively crossed over the mid-line.
Treatment involves taping, ultrasound, icing for pain relief as well as rehabilitation to strengthen your hip stabilising muscles.
4. Snapping hip
Snapping Hip Syndrome is a condition that is characterized by a snapping sensation, and/or audible “snap” or “click” noise, in or around the hip when it is in motion. For most people this condition is simply an annoyance; however it may result in both pain and weakness interfering with the patient’s functional mobility.
Causes :
1.External (most common)
⦁ Iliotibial band (or “ITB band”) snapping over the greater trochanter of the femur.

2.Internal
⦁ Iliopsoas tendon snapping over a bony prominence of the pelvis.
3.Intra-articular (least common)
⦁ Usually due to a tear of the cartilage and/or loose body within the hip joint that may also cause the hip to “lock up”.
Physiotherapy usually releases any tightness in the affected tendon and rehabilitates the weak structures of the hip causing the tightness. If conservative management fails then surgical intervention may be indicated.
 Tennis and Golfers elbow
Tennis and Golfers elbow
Tennis elbow has pain felt on the outside of the elbow and golfers elbow has pain felt on the inside of the elbow. Both are tendonopathies at the origin of the extensor or flexor muscles of the wrist.
This is typically an overuse injury, where an important aspect of the treatment is to find the cause and rehabilitate accordingly. A tendonitis becomes known as a tendonopathy as the pathology progresses.
Physiotherapy treatment may include joint mobilisation techniques of either the elbow joint, superior and inferior radio-ulnar joint. The cervical spine is often mobilised for a downward modulating affect on the nervous system to decrease pain. Neural sliders to improve neural mobility.
Myofacial release and deep dry needling may be used to release tightness in the muscles to decrease tension on the tendonous origin. Ice and ultrasound can be used for inflammation and Taping can be used to offload the affected tendon.
Strengthening will often include shoulder girdle exercises and a gradual loading of the affected tendon.
Shoulder pain has various causes; these are a few common injuries:
1.Shoulder tendonopathy is common in sports such as tennis, cricket, swimming, boxing and rugby. Tendons around the shoulder (the rotator cuff or long head biceps) can become inflamed (tendonitis) or torn, causing pain. Tendonpathies are also common in the elderly, especially if hobbies or work included lots of overhead activity or overuse.
2. Shoulder bursitis is an inflamed shoulder bursa. Your bursa is a fluid-filled sac that helps to reduce friction in your shoulder spaces. You have several bursae within your shoulder. Your subacromial bursa is the most commonly inflamed of the shoulder bursa. This condition is typically present together with shoulder impingement syndrome.
3. Shoulder impingement syndrome is common, especially as a lot of us have poor posture. Often an arc of pain is described and a feeling of catching in a certain range of movement in the shoulder. Shoulder pain can be felt in front or at the side of the shoulder. Often the shoulder on the affected side is found to be raised and rotated forward and if one looks at the shoulder blade it will be raised from the thorax on that side. Physiotherapists rehabilitation program is aimed at improving the position of the shoulder joint and the shoulder blade. Tight structures that resist this position are released with dry needling and, or deep massage; and the weak muscles are strengthened. Biomechanical taping can be used initially to place the shoulder joint in a better position to help decrease pain during the initial phase of rehabilitation.
4. A dislocated shoulder may be caused by a heavy fall or sudden impact. The upper arm painfully “pops” out of the shoulder joint and you won’t be able to move your arm. Once your doctor has confirmed there is no associated fracture or tendon rupture, and has relocated your shoulder then you will begin physiotherapy. A sling can be used initially to decrease pain- but you should not keep your shoulder still 24 hours a day.. you will then have other complications such as a stiff shoulder joint, increased pain experience, increased weakness and delayed rate of healing. The sling is there to rest your shoulder to decrease inflammation during the first phase of healing.
It is important to ice your shoulder the first 5-10 days after the injury.
Physiotherapy will help decrease pain, promote good healing, mobilise the shoulder to gain full range of motion. Biomechanical taping can be used to stabilise the shoulder and reduce pain. It is VERY important after this injury to strengthen your shoulder girdle especially your rotator cuff and anterior fibres deltoid. Strengthening is the most important thing that you can do to prevent the shoulder from dislocating again.
Recurrent shoulder dislocations can cause tears and arthritis of the shoulder over time.
Osteoarthritis of the knee
Osteoarthritis (OA) is the most commo n disease of joints adults suffer from worldwide.
n disease of joints adults suffer from worldwide.
Osteoarthritis of the knee most commonly affects a population age of 45 and older., and it is the joint most commonly affected by OA. This condition occurs gradually with age and the cartilage in the knee wears away eventually causing bone on bone contact between joint surfaces. Most common complaints include joint swelling, joint stiffness, and pain. Knee osteoarthritis can be diagnosed on x ray.
You get Primary and secondary OA. The difference is that primary OA is usually your normal age related degeneration, while your secondary OA is usually caused as a result of something else i.e. obesity, genetics, or a previous knee injury that was not rehabilitated properly and resulted in an unstable knee joint.
You can have knee osteoarthritis without having pain. If you are experiencing pain then you need to learn to manage your symptoms. During flare ups medication prescribed by your doctor can help manage your symptoms. It is a good idea to do what you can to offload your joint: this includes losing any extra weight you may be carrying, and strengthening the stabilising muscles around the knee joint. Exercise is very important to get that joint lubricating and to maintain mobility and strength. If you don’t move the joint often gets more stiff and the pain worsens. Your physiotherapist can help mobilise the knee joint and give advice on strengthening and mobilising exercise and activity modification to manage your lifestyle and pain.
A total knee replacement is only indicated in the last stage of knee OA (stage 4), when there is bone on bone contact. A total knee replacement is not as successful if it is done at an earlier stage, and your surgeon will usually wait.
If a total knee replacement is indicated then the physiotherapist will rehabilitate post operatively. The goals are to get you walking pain free again, to gain full range of motion of the knee post operatively, and to get you back to your previous function with strengthening of the hip and knee stabilisers post operatively, as these are very important in balance and a successful outcome. Your Quadriceps muscle strength is a good indicator of a successful outcome post operatively.
Sudden knee pain commonly involves twisting. It’s usually caused by a sprain, strain or tendonitis.
Other knee injuries include:
1.Runner’s knee/ chondromalacia – symptoms include soreness and discomfort beneath or to one side of your kneecap; it can also cause a grating sensation in your knee. Often the cause is a tight ITB, weak buttocks muscles and weak quadriceps- especially VMO. Physiotherapy will include releasing any tight structures, strengthening the muscles found to be weak and often taping to help reduce pain and realign the knee cap or to assist in activation of weak muscles during the rehabilitation process.
2. Cartilage damage – this can be gradual thinning of the cartilage or an acute tear of the cartilage (meniscus). Often symptoms include a ‘catching’ when straightening a bent knee or a feeling of the knee locking. Treatment includes reducing pain and strengthening the muscles around the knee to offload the knee joint. If one carries extra weight then usually one can reduce a lot of the symptoms if not all by losing some weight. Surgical intervention often includes an arthroscopy and debridement to clean out the joint. Post operatively the patient needs to strengthen the muscles around the knee and lose extra weight to have a successful outcome.
3. ITB friction syndrome– This pain is commonly felt on the outside of the knee. Cyclists and runners often suffer from this condition. It is an inflammatory condition driven by repetitive friction over the ITB and the lateral femoral condyle. The ITB is tight and needs to be released to reduce the friction over the lateral femoral condyle. The cause of the tight ITB is usually weakness of the Gluteus muscles. Physiotherapy usually includes myofascial release and or dry needling of the ITB, strengthening program of the muscles assessed to be weak and specific taping to reduce pain during the rehabilitation process.
4. Torn Anterior cruciate ligament (ACL) – this is usually with a twisting injury to the knee while the foot is planted firmly on the ground. Typically there is swelling and pain and one can’t put weight on that leg afterwards. This ligament is a significant stabiliser of the knee joint. An anterior drawer test is usually positive when the swelling has subsided- this will be assessed by your doctor or physiotherapist. A tear can be full or partial. Depending on your age and your physical activity an ACL repair may be done surgically. Usually if an athlete has a full tear then the ACL is surgically repaired. Post operatively the physiotherapist will help with pain control, gaining full range of movement of your knee and strengthening your lower quarter. Your Quadriceps strength has been found to be the most significant indicator of a successful outcome. If surgery is not done the physiotherapists role is the same as above.
5. Collateral ligament sprain or tear– These are found on the sides of your knee and help with stability of the knee. The medial or “inside” collateral ligament (MCL) connects the femur to the tibia. The lateral or “outside” collateral ligament (LCL) connects the femur to the smaller bone in the lower leg (fibula). The collateral ligaments control the sideways motion of your knee and brace it against unusual movement. The pain is usually felt on the side of the knee along the affected ligamant. Injury to the ligament is usually with a force to the knee stretching or tearing that ligament. Physiotherapy assists with reducing pain and improving range of motion at the knee as well as strengthening and taping to increase stability of the knee.
6. Dislocated patella (knee cap)- This is usually traumatic but can happen in people that have very lax ligaments or a shallow patella femoral groove for the patella to glide in. The kneecap slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place and usually found more to the outside of the knee. It is more common in young female athletes. If the knee cap only shifts partly out then it is known as a sublaxation and not a dislocation.
Physiotherapy is indicated to reduce pain and swelling, gain full range of motion of the knee and most importantly to strengthen the knee with special focus on VMO and Quadricep strengthening. Biomechanical taping can be used to stabilise the patella during the initial rehabilitation process. The strengthening is to prevent the patella from dislocating or sublaxing again. If a persons patella sublaxes and dislocates recurrently regardless of compliance to a good rehabilitation program then usually surgery is required and then physiotherapy is commenced post operatively again.
If a patella is left to keep dislocating, arthritis will occur over time, along with worsening and disabling pain after each dislocation.









