Sports injuries differ from everyday injuries. Athletes normally require a high level of performance and demand placed upon their body, which pushes their muscles, joints and bones to the limit. Sports physiotherapists help athletes recover from sports injuries, and provide education and resources to prevent injuries and help improve performance.
Your physiotherapist has sport-specific knowledge that addresses acute, chronic and overuse injuries.
Common sports injuries
This is the most common type of sports inju ry. The difference between a strain and a sprain is that a:
ry. The difference between a strain and a sprain is that a:
⦁ sprain happens when one or more of the ligaments are stretched, twisted or torn
⦁ muscle strain (“pulling a muscle”) happens when muscle tissues or fibres are stretched or torn.
Symptoms of a sprain or strain can include pain, swelling, bruising and tenderness around a joint or in a muscle. You may also find it difficult to move the affected body part.
An ankle sprain is one of the most common ankle injuries and can become recurrent if not rehabilitated properly the first time.
 Back pain is usually caused by a sprain or strain in the back. Warming up properly before exercise can reduce the risk of back pain.
Back pain is usually caused by a sprain or strain in the back. Warming up properly before exercise can reduce the risk of back pain.
Back pain is often felt as soreness, tension or stiffness in the lower back, but it can be felt anywhere from the neck and shoulders down to the buttocks and legs.
Physiotherapists assess the cause of your back pain and then use various treatment techniques to alleviate pain, improve mobility and to strengthen your back.
It is important to keep moving when you have back pain. A maximum of 2 days bed rest is allowed when pain is too severe to move. Moving will keep the spine and nerves lubricated, and provide blood and oxygen supply to the spine, ligaments, discs and muscles. Remember any tissue that is healing heals quicker with better blood supply. Your physiotherapist can provide you with some exercises that should help alleviate your pain in the beginning.
Physiotherapy may consist of myofacial/ trigger point release, pain education, spinal mobilisation, neural mobilisation, deep dry needling, electrotherapy, ice/heat, taping and specific exercises.
 Repetitive activity or a heavy impact while playing sport can injure bones, causing:
Repetitive activity or a heavy impact while playing sport can injure bones, causing:
⦁ stress fractures – bone pain caused by tiny cracks that develop in a bone as a result of repeated stresses (for example, during high-impact activities like distance running)
⦁ shin splints – painful shins caused by inflammation in the tissues surrounding the shin bone; it’s common in sports that involve running
⦁ a broken ankle, wrist, arm, leg, toe or finger.
A broken bone may cause swelling, significant bruising and tenderness around the injured area, and bleeding if the bone has broken the skin (an open fracture). It’s unlikely you’ll be able to use the affected limb. In this case you will need to see your Doctor, and physiotherapy is only indicated in certain cases once the bone has healed for rehabilitation to make sure there is good flexibility, proprioception and strength around the affected area. Physiotherapy will also help for pain and swelling. Occasionally in the case of an undisplaced ankle fracture where you may be put in a moon-boot for 6 weeks- physiotherapy can be commenced earlier to reduce pain and swelling with methods such as taping, oedema massage, ice and the introduction of safe exercises.
 Hamstrings are commonly injured when an athlete uses sudden explosive energy to run, jump, lunge or push off. This could result in a sprain, strain or muscle tear of the belly of the hamstring muscle. This can be felt or heard as a pop and will be immediately painful. The muscle will spasm and feel tight and tender. In some cases, there may also be swelling and bruising.
Hamstrings are commonly injured when an athlete uses sudden explosive energy to run, jump, lunge or push off. This could result in a sprain, strain or muscle tear of the belly of the hamstring muscle. This can be felt or heard as a pop and will be immediately painful. The muscle will spasm and feel tight and tender. In some cases, there may also be swelling and bruising.
Another common hamstring injury is a hamstring tendonopathy which is usually due to repetitive overuse. It can often be felt at it’s origin just deep to the buttocks and often only felt after exercise with pain reducing with exercise initially. As the condition progresses it can be felt throughout exercise and finally you will feel it even at rest. This condition is better treated in the beginning stages. Tendonopathies are notoriously difficult to treat when they have been there for a long time.
Physiotherapists decrease pain and rehabilitate. Special focus is on eccentric strengthening of the hamstring.
1. Concussion is a common head injury especially in contact sports such as rugby.
Please see a doctor immediately if a concussion is suspected. These are some of the signs and symptoms:
⦁ unconsciousness (even if it was only very brief)
⦁ difficulty staying awake or still being sleepy several hours after the injury ⦁ disorientation
⦁ disorientation
⦁ a seizure or fit
⦁ difficulty speaking, such as slurred speech
⦁ significantly blurred vision or double vision
⦁ difficulty understanding what people say
⦁ vomiting
2. Whiplash injury
If you have sustained a concussion, the force will always be significant enough to cause an associated whiplash injury.
 As physiotherapists we are well trained in treating whiplash injuries. For the first 48 hours it is important to ice your neck following a whiplash injury for the inflammation. It is also VERY important to move your neck so that your joints in your neck lubricate and glide properly when you move and that you maintain good blood supply in the area. If you keep your neck still (or in a soft collar) you often aggravate the pain and slow the healing process down. Your physiotherapist will evaluate your spine and mobilise any stiff joints, release tight muscle spasms with deep tissue
As physiotherapists we are well trained in treating whiplash injuries. For the first 48 hours it is important to ice your neck following a whiplash injury for the inflammation. It is also VERY important to move your neck so that your joints in your neck lubricate and glide properly when you move and that you maintain good blood supply in the area. If you keep your neck still (or in a soft collar) you often aggravate the pain and slow the healing process down. Your physiotherapist will evaluate your spine and mobilise any stiff joints, release tight muscle spasms with deep tissue
massage and sometimes dry needling. They will give you exercises for mobilisation and strengthening of your neck to regain previous function and to prevent chronic neck pain or headaches following a whiplash injury.
 Heel pain can occur when the thick band of tissue that runs under the sole of the foot becomes inflamed. It’s common in runners and is called plantar fasciitis. Although you don’t need to be an athlete to suffer from this condition.
Heel pain can occur when the thick band of tissue that runs under the sole of the foot becomes inflamed. It’s common in runners and is called plantar fasciitis. Although you don’t need to be an athlete to suffer from this condition.
It can cause a sharp and often severe pain when you place weight on your heel. It is often worse in the mornings when you wake up. In most cases, only one heel is affected, although some people have pain in both heels. Tight calves and shoes that don’t support the arch of your foot properly have been found to contribute to the development of this condition.
Heel pain and stiffness can also sometimes be caused by tendonopathy or tightness of the Achilles tendon, which runs up the back of the heel. This can occur gradually over a long period of time, or the tendon can suddenly rupture or tear.
Another cause of heel pain can be a stress fracture due to repetitive load in sports such as running, although most fractures of the heel are caused traumatically from a fall landing on the heel.

Swollen joints can be caused by conditions that affect the joints or structures around joints, such as bursa and tendons. Bursa are small fluid-filled sacs underneath the skin, found over the joints and between tendons and bones which reduce friction when moving.
Examples of these types of conditions include:
bursitis – a swollen bursa; bursitis is common in the knee, hip and elbow. A bursa is supposed to decrease friction between a tendon and bone, but can become inflamed and cause severe pain. This is often due to a mechanical overload at that area and along with pain management one will need to strengthen and stretch certain muscles that are causing this overload to have a long term benefit.
Tendonitis – an enlarged tendon around the shoulder (rotator cuff/ bicep), elbow (tennis elbow/ golfers elbow), wrist (dequervins tenosynovitis), thigh(hamstring), knee ( patella tendon) or back of the heel(achilles tendon) This is typically also an overuse injury, where an important aspect of the treatment is to find the cause and rehabilitate accordingly. A tendonitis becomes known as a tendonopathy as the pathology progresses.
Sudden knee pain is common in contact sports, particularly those that involve twisting. It’s usually caused by a sprain, strain or tendonitis.
Other knee injuries include:

1. Runner’s knee/ chondromalacia – symptoms include soreness and discomfort beneath or to one side of your kneecap; it can also cause a grating sensation in your knee. Often the cause is a tight ITB, weak buttocks muscles and weak quadriceps- especially VMO. Physiotherapy will include releasing any tight structures, strengthening the muscles found to be weak and often taping to help reduce pain and realign the knee cap or to assist in activation of weak muscles during the rehabilitation process.
2. Cartilage damage – this can be gradual thinning of the cartilage or an acute tear of the cartilage (meniscus). Often symptoms include a ‘catching’ when straightening a bent knee or a feeling of the knee locking. Treatment includes reducing pain and strengthening the muscles around the knee to offload the knee joint. If one carries extra weight then usually one can reduce a lot of the symptoms if not all by losing some weight. Surgical intervention often includes an arthroscopy and debridement to clean out the joint. Post operatively the patient needs to strengthen the muscles around the knee and lose extra weight to have a successful outcome.
3. ITB friction syndrome – This pain is commonly felt on the outside of the knee. Cyclists and runners often suffer from this condition. It is an inflammatory condition driven by repetitive friction over the ITB and the lateral femoral condyle. The ITB is tight and needs to be released to reduce the friction over the lateral femoral condyle. The cause of the tight ITB is usually weakness of the Gluteus muscles. Physiotherapy usually includes myofascial release and or dry needling of the ITB, strengthening program of the muscles assessed to be weak and specific taping to reduce pain during the rehabilitation process.
4. Torn Anterior cruciate ligament (ACL) – this is usually with a twisting injury to the knee while the foot is planted firmly on the ground.

Typically there is swelling and pain and one can’t put weight on that leg afterwards. This ligament is a significant stabiliser of the knee joint. An anterior drawer test is usually positive when the swelling has subsided- this will be assessed by your doctor or physiotherapist. A tear can be full or partial. Depending on your age and your physical activity an ACL repair may be done surgically. Usually if an athlete has a full tear then the ACL is surgically repaired. Post operatively the physiotherapist will help with pain control, gaining full range of movement of your knee and strengthening your lower quarter. Your Quadriceps strength has been found to be the most significant indicator of a successful outcome. If surgery is not done the physiotherapists role is the same as above.
5. Collateral ligament sprain or tear – These are found on the sides of your knee and help with stability of the knee. The medial or “inside” collateral ligament (MCL) connects the femur to the tibia. The lateral or “outside” collateral ligament (LCL) connects the femur to the smaller bone in the lower leg (fibula). The collateral ligaments control the sideways motion of your knee and brace it against unusual movement. The pain is usually felt on the side of the knee along the affected ligamant. Injury to the ligament is usually with a force to the knee stretching or tearing that ligament. Physiotherapy assists with reducing pain and improving range of motion at the knee as well as strengthening and taping to increase stability of the knee.
6. Dislocated patella (knee cap) – This is usually traumatic but can happen in people that have very lax ligaments or a shallow patella femoral groove for the patella to glide in. The kneecap slips out of its normal position. Often the knee is partly bent, painful and swollen. The patella is also often felt and seen out of place and usually found more to the outside of the knee. It is more common in young female athletes. If the knee cap only shifts partly out then it is known as a sublaxation and not a dislocation.
Physiotherapy is indicated to reduce pain and swelling, gain full range of motion of the knee and most importantly to strengthen the knee with special focus on VMO and Quadricep strengthening. Biomechanical taping can be used to stabilise the patella during the initial rehabilitation process. The strengthening is to prevent the patella from dislocating or sublaxing again. If a persons patella sublaxes and dislocates recurrently regardless of compliance to a good rehabilitation program then usually surgery is required and then physiotherapy is commenced post operatively again.
If a patella is left to keep dislocating, arthritis will occur over time, along with worsening and disabling pain after each dislocation.
 1. Shoulder tendonopathy is common in sports such as tennis, cricket, swimming, boxing and rugby. Tendons around the shoulder (the rotator cuff or long head biceps) can become inflamed (tendonitis) or torn, causing pain.
1. Shoulder tendonopathy is common in sports such as tennis, cricket, swimming, boxing and rugby. Tendons around the shoulder (the rotator cuff or long head biceps) can become inflamed (tendonitis) or torn, causing pain.
2. Shoulder bursitis is an inflamed shoulder bursa. Your bursa is a fluid-filled sac that helps to reduce friction in your shoulder spaces. You have several bursae within your shoulder. Your subacromial bursa is the most commonly inflamed of the shoulder bursa. This condition is typically present together with shoulder impingement syndrome.
3. Shoulder impingement syndrome is also common in athletes who use there shoulder repetitively above there head. Often an arc of pain is described and a feeling of catching in a certain range of movement in the shoulder. Shoulder pain can be felt in front or at the side of the shoulder. Often the shoulder on the affected side is found to be raised and rotated forward and if one looks at the shoulder blade it will be raised from the thorax on that side. Physiotherapists rehabilitation program is aimed at improving the position of the shoulder joint and the shoulder blade. Tight structures that resist this position are released with dry needling and, or deep massage; and the weak muscles are strengthened. Biomechanical taping can be used initially to place the shoulder joint in a better position to help decrease pain during the initial phase of rehabilitation.
4. A dislocated shoulder may be caused by a heavy fall or sudden impact. The upper arm painfully “pops” out of the shoulder joint and you won’t be able to move your arm. Once your doctor has confirmed there is no associated fracture and has relocated your shoulder then you will begin physiotherapy. A sling can be used initially to decrease pain- but you should not keep your shoulder still 24 hours a day.. you will then have other complications such as a stiff shoulder joint, increased pain experience, increased weakness and delayed rate of healing. The sling is there to rest your shoulder to decrease inflammation during the first phase of healing.
It is important to ice your shoulder the first 5-10 days after the injury.
Physiotherapy will help decrease pain, promote good healing, mobilise the shoulder to gain full range of motion. Biomechanical taping can be used to stabilise the shoulder and reduce pain.
 It is VERY important after this injury to strengthen your shoulder girdle especially your rotator cuff and anterior fibres deltoid. Strengthening is the most important thing that you can do to prevent the shoulder from dislocating again.
It is VERY important after this injury to strengthen your shoulder girdle especially your rotator cuff and anterior fibres deltoid. Strengthening is the most important thing that you can do to prevent the shoulder from dislocating again.
Recurrent shoulder dislocations can cause tears and arthritis of the shoulder over time.
1. Ankle sprain– this is a common injury that often occurs when one twists ones ankle. It is often the outside ligaments that are injured. The ligaments of the ankle give the ankle stability. The severity of an ankle sprain depends on whether the ligament is stretched, partially torn or completely torn, as well as on the number of ligaments involved.
Physiotherapy is important to decrease pain and swelling and to maintain flexibilty as well as to rehabilitate important muscles such as posterior tibialis to improve stability of the ankle.

It is also important to have your balance and proprioception rehabilitated to prevent reinjury.
2. Achilles Tendonopathy– is a common overuse injury caused by repetitive energy storage and release with excessive compression. This can lead to a sudden injury, or in the worst case, can cause a rupture of the Achilles tendon. In both cases, a lack of flexibility or a stiff Achilles tendon can increase the risk of these injuries. We often find a weak glut max to be a contributing factor as well. Achilles tendinopathy can be described as insertional or mid portion, the difference is in the localisation. The insertional form is situated at the level of transition
 between the Achilles tendon and the bone, the midportion form is located at the level of the tendon body. Physiotherapists release the tight calf muscle, and begin a gradual loading program of the tendon that doesn’t cause inflammation of the tendon but that stimulates placement of new good and healthy tendon. Strengthening of any other muscles found to be weak is commenced. Taping and advice on shoes can be of value to decrease pain during the rehabilitation process.
between the Achilles tendon and the bone, the midportion form is located at the level of the tendon body. Physiotherapists release the tight calf muscle, and begin a gradual loading program of the tendon that doesn’t cause inflammation of the tendon but that stimulates placement of new good and healthy tendon. Strengthening of any other muscles found to be weak is commenced. Taping and advice on shoes can be of value to decrease pain during the rehabilitation process.
3. Anterior impingement syndrome– Anterior Ankle Impingement is a condition where an individual experiences pain at the front of the ankle, due to compression of the bony or soft tissue structures during activities that involve maximal ankle dorsiflexion motion. Symptoms often worsen with activities such as a deep squat, stretching of the calf, running (especially uphill), and landing from a jump. Often there is a puffiness seen on top of the ankle. Treatment includes rest and icing. Your physiotherapist may mobilise your talus bone of the ankle and release tibialis anterior which may be tight to reduce the impingement. Often poor rehabilitation after a previous ankle sprain predisposes a person to this condition. General rehabilitation of the lower leg will be included to strengthen any weak muscles.






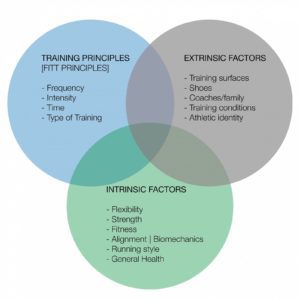
What places the athlete at risk for injury?
It is usually a combination of three groups of factors, some are changeable and others need to be considered as they remain relatively fixed and make us unique.